Parkinson’s Disease
What is Parkinson’s disease?
Parkinson’s disease is a progressive neurological disorder characterised initially by movement-related issues. These movements rely on dopamine, a neurotransmitter produced in the substantia nigra of the brain. In Parkinson’s, the degeneration of substantia nigra cells leads to a reduction in dopamine levels, triggering symptoms once levels drop by 60 to 80 per cent.
What are some misconceptions associated with Parkinson’s disease?
Although this disease is often seen in elderly persons, it is not typical for ageing.
What are the Symptoms of Parkinson’s disease?
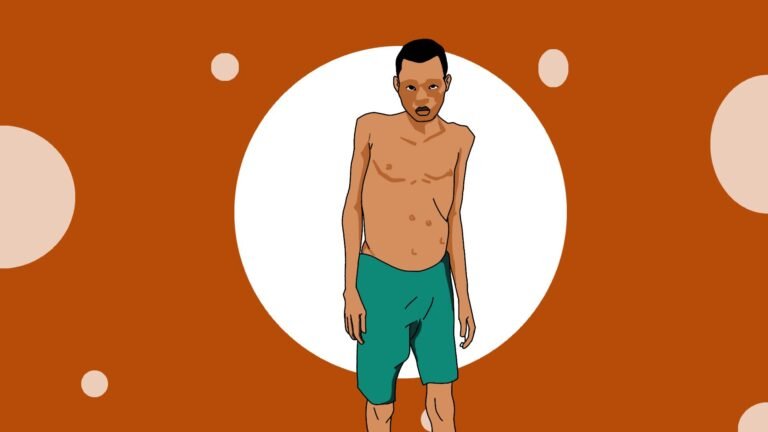
Early signs of Parkinson’s can manifest years before motor symptoms develop, including decreased sense of smell (anosmia), constipation, small handwriting (micrographia), voice changes, and stooped posture. The primary motor symptoms include tremors, slow movements (bradykinesia), stiffness of limbs and trunk (rigidity), and difficulties with balance and falling.
Secondary symptoms include a blank facial expression, freezing while walking, soft and muffled speech, decreased blinking and swallowing, a tendency to fall backwards, reduced arm swing during walking, and a shuffling gait known as Parkinsonian. Other associated symptoms may involve seborrheic dermatitis (flaky scales on oily skin areas), an increased risk of melanoma (skin cancer), and sleep disturbances such as vivid dreams, talking, and movement during sleep.
What are the causes of Parkinson’s disease?
The precise origin of Parkinson’s disease remains elusive, yet it is thought to result from a blend of genetic and environmental influences. Although specific triggers are not fully understood, several factors have been recognised as potential contributors to the condition:
- Sex: Men are about one and a half times more likely to develop Parkinson’s disease as compared to women.
- Race: Research indicates a higher prevalence of Parkinson’s disease among white individuals compared to Black or Asian populations. Geographic location may contribute to this disparity.
- Age: Parkinson’s disease typically manifests between 50 and 60 years old. It rarely occurs before age 40, affecting only about four per cent of cases.
- Family History: There is an increased risk of Parkinson’s in individuals with a family history of Parkinson’s disease.
- Toxins: Exposure to certain environmental toxins has been linked to an elevated risk of Parkinson’s disease.
- Head Injury: People who have experienced significant head injuries may have a higher likelihood of developing Parkinson’s disease later in life.
These factors contribute to the complex interplay of genetics and environmental influences that underlie the onset and progression of Parkinson’s disease.
How is Parkinson’s disease diagnosed?
Diagnosing Parkinson’s disease typically involves a thorough assessment rather than a specific diagnostic test. Healthcare providers rely on medical history, physical and neurological examinations, and a detailed review of signs and symptoms. Imaging tests like CT scans or MRIs may be employed to help rule out other conditions that could present with similar symptoms to Parkinson’s. These tests can provide valuable information about the brain’s structure and rule out other potential causes for the symptoms observed.
Ultimately, diagnosing Parkinson’s disease is based on clinical judgment and the presence of characteristic motor and non-motor symptoms that are consistent with the condition.
What is the treatment for Parkinson’s disease?
Treatment for Parkinson’s disease involves a multifaceted approach that combines lifestyle changes, medications, and various therapies aimed at managing symptoms and improving quality of life. Here’s an overview of the critical components of treatment:
Lifestyle Changes
- Adequate Rest: Ensuring sufficient sleep is crucial as fatigue is common in Parkinson’s.
- Regular Exercise: Physical activity helps maintain mobility, balance, and well-being.
- Balanced Diet: Eating nutritious meals supports general health and can improve medication effectiveness.
Medications
- Parkinson’s disease medications primarily aim to replenish dopamine levels or mimic its effects in the brain. The main types include:
- Levodopa (often combined with carbidopa): This is the most effective medication for Parkinson’s as it directly replenishes dopamine levels in the brain, alleviating motor symptoms like tremors and rigidity.
- Dopamine Agonists: Drugs such as bromocriptine, pramipexole, and ropinirole mimic the action of dopamine in the brain. They are often used alongside or as an alternative to levodopa.
- Anticholinergics: Medications like benztropine and trihexyphenidyl can help manage tremors and rigidity by blocking the effects of acetylcholine, a neurotransmitter that can worsen these symptoms.
- Amantadine: This medication can provide short-term relief for dyskinesia caused by involuntary movements that can be a side effect of levodopa treatment.
Therapies
- Speech Therapy: Helps improve communication abilities affected by changes in speech and swallowing.
- Occupational Therapy: Focuses on maintaining independence in daily activities like dressing and eating.
- Physical Therapy: Exercises and techniques to improve mobility, balance, and flexibility.
Parkinson’s surgery
Surgical interventions for Parkinson’s disease are typically considered for individuals who do not adequately respond to medication, therapy, and lifestyle modifications. There are two main types of surgical procedures used to treat Parkinson’s:
- Deep Brain Stimulation (DBS) involves implanting electrodes into the specific areas of the brain controlling movement. These electrodes are connected to a pulse generator (like a pacemaker), which emits electrical impulses to regulate abnormal brain activity and alleviate symptoms such as tremors, rigidity, and dyskinesia.
- Pump-Delivered Therapy: This approach involves implanting a device called a pump under the skin of the abdomen. The pump delivers a continuous medication infusion directly into the spinal fluid, bypassing the digestive system and allowing for more consistent symptom control. This method particularly benefits individuals who experience fluctuations in their response to oral medications.
These surgical options are considered when Parkinson’s symptoms significantly impair daily functioning despite optimal medical management. Each procedure carries its benefits and risks, and the decision to undergo surgery is usually made in consultation with a neurologist and neurosurgeon after carefully evaluating the individual’s specific symptoms and medical history.